Everyday Functioning & Outcomes in Heart Failure
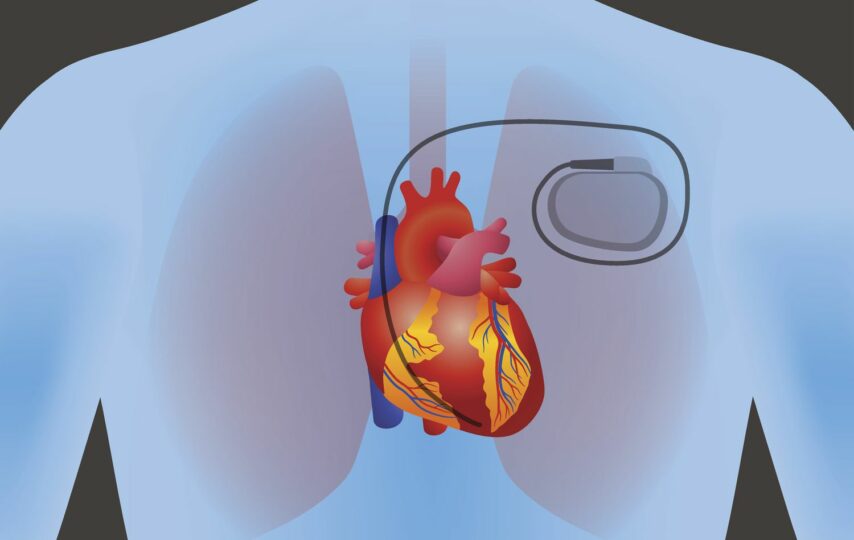
Some heart blockage symptoms include light-headedness, fainting, fatigue, and difficulty breathing. An implantable pacemaker is a frequent therapeutic option.
Heartbeat
The heart muscle contracts with each heartbeat to circulate blood throughout the body. A senatorial node is a group of specialised cells responsible for producing the electrical impulses that set off the contractions (SA node). Since it produces electrical impulses at regular intervals like mechanical pacemakers, the SA node has earned the nickname “natural pacemaker.”
If there is a barrier in the pathway from the AV node to the ventricles, the heart will not receive an electrical impulse. Even if the heart muscle stops during a heart block, the body has various “backup” mechanisms that may keep the blood pumping. Yet, this condition may cause the heart to beat slowly (bradycardia), which depletes oxygen from the blood and harms the body’s organs and tissues.
How Serious Is It?
The severity of heart block varies from case to case. Many patients with heart blockage symptoms or Type I heart block (including both first- and second-degree heart blocks) need no therapy. There may be minimal effect on your health and quality of life from these forms of heart block in the end.
You will likely require a pacemaker if you have heart blockage symptoms of the second or third degree (Type II or III). Still, by making certain modifications to your lifestyle, you may improve your quality of life and extend the time you can remain independent. In very unusual circumstances, a pacemaker may be necessary for individuals with heart block and who suffer from syncope (regular bouts of fainting).
Heart failure is a major risk factor for those with heart block. According to research published in 2018, those with full heart block are more likely to develop heart failure. Organ failure and sudden death are additional risks associated with third-degree heart block (no heartbeat).
Heart Block Types
The ventricles nevertheless receive all electrical impulses, although slowly, in first-degree heart block. Most people with first-degree heart block will never experience any symptoms and will not need therapy. Intense training may lead to a sluggish resting heart rate, which increases the risk of developing a heart block.
Second-degree types of heart block occur when electrical impulses are delayed with each heartbeat to the point that a beat does not reach the ventricles. Dizziness and other symptoms may be experienced by those with second-degree heart block, which may eventually need medical intervention.
Complete types of heart block, or heart block of the third degree, is a life-threatening condition. In a normal heart, electrical signals from the atria never reach the ventricles. The ventricles may generate electrical impulses to set off ventricular escape beats if they aren’t getting any from the heart’s electrical system. They are the heart’s backup beats and are usually rather sluggish. Third-degree heart block may cause symptoms including fainting, dizziness, and exhaustion. Third-degree heart block is potentially lethal if not addressed.
What Methods Exist For Identifying Heart Block?
Physical examinations that do not involve a stethoscope listening to the heart are incomplete. Your symptoms, prescriptions, and supplements, as well as your personal and family medical history, should all be taken into account.
A normal physical examination and electrocardiogram (ECG) may typically identify first-degree treating heart block and even some instances of second-degree heart block. Electrocardiograms (ECGs) are a non-invasive method of gauging the heart’s intensity, pace, and rhythm of electrical activity using electrodes.
Electrophysiology studies, which include inserting a catheter into a blood artery, may be ordered by your doctor in very unusual circumstances. The next step involves directing the catheter towards the heart to record electrical signals from the organ.
What Percentage Of People Experience Heart Blocks?
While infrequent, heart blockages of the first degree and Mobitz type 1 occur. According to estimates, between 0.5% and 2% of otherwise healthy persons have complete heart blockages.
Those with certain cardiac problems are more likely to develop Mobitz type 2 heart block than the general population. Mobitz type 2, for instance, is thought to affect 1 in 30 persons who already have heart failure.
One in every 20,000 infants is affected with congenital third-degree heart block. Contrarily, developed third-degree heart block is a frequent consequence of cardiac disease, especially in the elderly. Third-degree causes of heart block are thought to affect 5-10% of the elderly with a cardiac history over 70.
How Serious Or Life Threatening Is Heart Block?
Indeed, that is possible. Individuals may have heart block in different places, at different intensities, and with a wide range of symptoms. Severe heart block, if ignored, may lead to abrupt cardiac arrest (the heart stops beating) but usually causes of heart block dizziness and fainting.
Conclusion
Your pacemaker will need to be evaluated regularly to ensure that it is still functioning properly by your cardiologist. Both remote and in-person assessments are used in the monitoring process. Mobile phone networks, including Bluetooth and Wi-Fi, are used for remote monitoring.
This facilitates near-constant monitoring by your doctor’s office. Furthermore, once a year, you will need to schedule an in-person appointment for treating heart block. To ensure your pacemaker is controlling your pulse properly, you must follow your doctor’s recommendations for monitoring.